08 Feb Osteoarthritis of the Knee is not a Death Sentence
Having osteoarthritis (OA) of the knee is not a death sentence. This long-ish post (resist the TL;DR!) should educate and inspire you if you have OA of the knee.
It’s not a death sentence for exercise, for sport, or for being able to do your daily activities independently. And for the countless young people we’ve come across that also have this diagnosis, it’s not the end of the world. But, you have to be smart about your lifestyle.
Which camp do you fall into?
- I have OA in my knee(s). If I exercise it will create further damage and therefore, pain. OR
- I have OA in my knee(s) and I exercise to lessen the pain and symptoms, strengthen the muscles surrounding the knee and improve my quality of life.
Which do you think is correct?
If you’re in Camp Number 2, YOU ARE CORRECT.
Camp Number 1 DOES NOT EXIST.
Read on to learn what you SHOULD do if you have OA of the knee.
Exercising with osteoarthritis of the knee should be commonplace, and not so controversial. Unfortunately, between, drugs, surgery, and other invasive and expensive interventions, we often overlook the few things that are within your control as remedies for the pain and lack of motion that often come with OA of the knee. Every physician, therapist, and trainer who works with osteoarthritis has the same creed: do no harm. With that, we work conservatively first, and only after that fails, do we advance to less conservative, more invasive options like drugs and surgery. Conservative treatment is where we start.
Getting people with osteoarthritis who have never exercised, who have “bad knees”, and who are symptomatic, to exercise is hard. Like, Really Hard! There’s a vicious cycle you all have probably heard about or experienced that loosely goes like this:
- You’ve lived with pain and stiffness, and for that reason, you don’t move much – because it hurts to move.
- You start an exercise program and with the addition of “some” range of motion and some strength building, you start to feel better – you have better range of motion, and feel stronger!
- You get excited and push exercise more, but maybe too much. Now you have swelling and more pain.
- So you stop moving. Your knee stiffens up, and you’re back in the cycle of not moving it because you’re afraid it’ll hurt.
- Rinse and Repeat!
While this cycle looks different to everyone, you get the point. Motion IS lotion, and in more ways than we ever knew. That simple phrase: “motion is lotion” IS TRUE! Not only does movement stimulate synovial fluid, the viscous gooey-like substance that bathes the inside of your knee and helps the joint glide more easily, and help the joint move better, but it also decreases inflammatory markers and increases anti-inflammatory processes. We’re learning so much more about how movement benefits our joints and our entire body that it is not only irresponsible to seek invasive and dangerous solutions but it’s insane. And by “dangerous” we mean prematurely choosing aggressive treatment over conservative lifestlye changes and exercise. In Invictus, William Earnest Henley says “I am the master of my fate, the captain of my soul”. You are the master of your fate. Your decisions regarding your health start with YOU….and only you. You decide. Those on your health care team advise, but you have a choice. Exercise is good! It’s the right first line of defense (along with maintaining ideal body weight, but we won’t go there in this post). The right type of exercise and the right dose (very important!) can yield unbelievable results. But yes, there are still choices to be made about WHAT exercise. Read on….
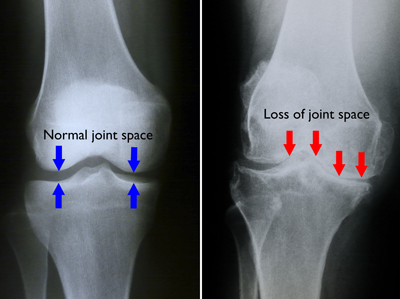
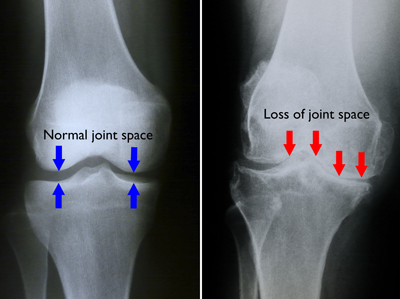
This graph from the CDC indicates increases in our population for arthritis in general. The growth is astounding, but if we realize our population is aging, it makes sense. Statistics show that 27 million Americans over the age of 60 have some OA of the knee. The causative factors of OA are still being researched. While we used to think of it as “wear and tear”, new research points to many more and complicated reasons a person may develop osteoarthritis. Here, we’re not addressing OA from an injury or as a result of a meniscal or ACL repair (or other surgical intervention) where the surgery predisposes the person to early-onset arthritis. Rather, we’re speaking to the gradual onset of arthritis, and what can be a debilitating condition.
We want to change the landscape of thought on osteoarthritis.
If you have it, then you have it. Perhaps major advances in science and technologies like stem-cell will someday be the norm, but for now, we’re rooted in the basics and believe that we should “clean up the house” before we decorate or renovate. In other words, let’s make sure all our health ducks are in a row that may make the symptoms of arthritis worse, and work through lifestyle changes and conservative therapies before we go under the knife or elect to take a new drug without serious consideration for future and long term side effects.
ABOUT THE KNEE
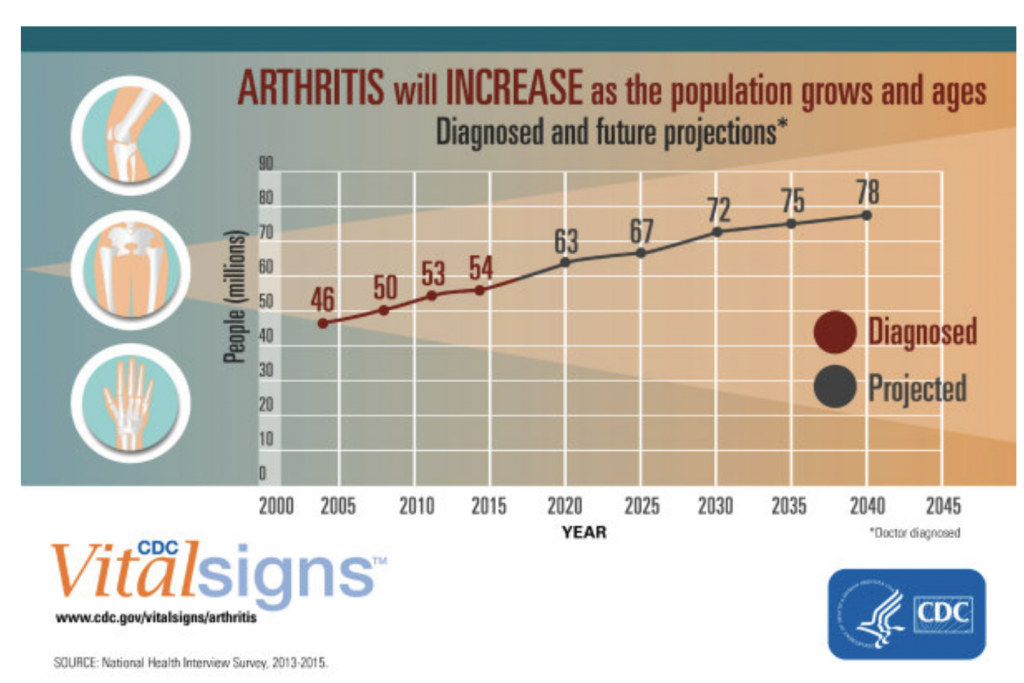
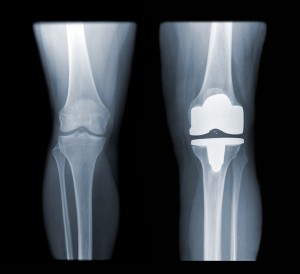
The knee is the largest joint in the body. It is a weight-bearing joint used in such simple, yet critical, tasks as walking, standing up from a chair, and bending to pick something up off of the floor (yes, the knee usually bends to the degree the person will allow in this movement). The knee is also the number one joint worldwide that is surgically reconstructed with a Total Knee Replacement (TKR). The image above is an X-ray of a normal knee and a Total Knee Replacement. This joint is kind of a big deal!
The knee has three “compartments”:
- the medial compartment, or the inside of the knee,
- the lateral compartment, or the outside of the knee,
- and the anterior or patellofemoral compartment, or the front of the knee under the kneecap.
Traditionally, based on the angulation of the legs at the hip and knee, we can tell “where” a person may experience arthritis-related symptoms. A person who is knock-kneed (also known as valgus) will usually experience symptoms in the lateral component. A person who is bow-legged (varus) will usually experience symptoms in the medial compartment. And if you add additional body weight to this picture, the symptoms are generally worse. Understanding the compartments and symptoms of an arthritic knee helps in creating an exercise program.
RANGE OF MOTION
The knee extends, flexes, and rotates somewhat.
- Knee extension is straightening your knee out all the way. “Full” extension is what we’re looking for. Often with arthritis, we’re lacking full knee extension.
- Knee flexion is bending your knee. “Full” flexion is approximately 140 degrees, although many people can do most activities of daily living with 125 degrees. When you have OA of the knee, often full flexion is painful, especially when weight-bearing. So we tend to avoid bending our knees…creating that vicious cycle we mentioned above. Lack of motion begets lack of motion. Here we go again!
- Regarding rotation – the knee joint is a modified hinge joint because there is “some” rotation that occurs, though not like that to the hip or shoulder. We’re not going to venture much down this rabbit hole today, but we wanted to acknowledge that “it rotates”.
Both knee flexion and extension are important to have in a healthy knee. Additionally, there is a small amount of femoral (the femur is the long leg bone above the knee) rotation on the tibia at the end ranges of extension – called the “screw home mechanism” – which is also important.
In an arthritic knee, we are cautious but work on improving these ranges of motion as they’re critical for functional movement. We define functional movements as movements that are based on real-life situational movements. Functional movements are usually multi-joint, and often multi-directional movements that place a demand on the body’s core, muscular and nervous systems. That was a lot, right? It is, but functional movements ARE complicated; complicated, but necessary.
MOVEMENT
Your knee, arthritic or not, needs to bend to sit down, and needs to extend to stand up and walk, at a minimum. Sitting, standing, and walking are functional movements. Your knee is a weight-bearing joint and functional movements for the knee are always weight-bearing. (Think not? challenge us!)
The stronger the muscles around your knee are, the more support they provide to that joint. Those muscles include your quadriceps (the front of your leg), your hamstrings (the back of your leg), your calf muscles: gastrocnemius and soleus (the lower leg), and your glutes (the butt).
The ankle is also a consideration because when we move the knee less, the ankle can lose mobility, and loss of ankle mobility can also prevent good movement of the knee.
FOUR REASONS YOU MUST EXERCISE AN ARTHRITIC KNEE
Motion is lotion. It’s true – we’ll tell you why.
Muscle facilitation. Sometimes muscles just don’t work right. We could give you volumes of sciency-reasons and opinions as to why, but let’s just park it here that sometimes they don’t work right, or they don’t work right in the right order. Our biggest three reasons are:
- They could have been ignored (you’ve been sedentary), or
- They’ve compensated for another problem so they’re malfunctioning, or
- Metabolically you have things going on that have broken that system
There are numerous reasons you may need to work on some muscle facilitation to either make your muscles work better or “turn them back on” if they are inhibited. The right type of movement can do this. You don’t always need expensive equipment or an actual rehabilitation clinic – and this is coming from a physical therapist! The right movement can facilitate muscles to work correctly and reconnect them to the brain and neurological system so they wake up.
Muscle strength. More than not, seniors are too sedentary. What is “too sedentary”? Well, in a 24-hour day, if 8 hours is sleep, we have 16 hours left. How many of those 16 hours are also (like sleep) not mobile hours? Half of them? In our opinion, it’s more than half. And while sitting to read a book, or the newspaper, or watch a television show is certainly a normal thing to do – is it normal for 8 hours? We think not. So, within that 16 hours, how are you moving, and how are you getting stronger? By not moving, you’re not only NOT getting stronger, but you’re getting weaker – for sure. At “our age” we have to work harder to stay strong. And lack of strength or muscle mass (sarcopenia) is a major contributor to and predictor of all-cause mortality over all other “diseases”. But, back to the knee, lack of strength in the lower extremity leads to balance problems, gait problems, and knee pain. Boom! There you have it. More strength almost always equals less pain.
Joint mobility and tissue pliability. Joint mobility goes without saying – the more you move a joint the more it moves. We see it every day in the shoulder – a person never moves it because it hurts. We start moving it in pain-free ranges and the pain-free range gets larger and larger and before you know it, we have full range without pain. It’s no exception in the knee. Moving it – correctly and cautiously, in functional patterns is not only productive, but it’s necessary.
Now, imagine that knee that isn’t moving because it hurts. The muscles surrounding the knee that we mentioned above are also not moving. They’re not contracting, they’re not lengthening…they’re getting stiff, fibrous, and beginning to lack the pliability they need to help that knee move and support it. Not only does moving the knee benefit the joint, but it benefits the muscles, tendons, and ligaments surrounding the joint. And don’t get us going on the blood flow and fluid movement when you don’t move a limb! That’s for another post.
Posture. Lastly, when you stop moving your knee correctly, lots of things happen. Your gait changes, compensation occurs and your posture can change. People who can’t or don’t straighten their knees all the way may begin walking with a more flexed hip, or they may lean back and “hang on their hip flexors” more. While problems “downstream” in the ankle and foot can cause problems in the knee, and problems upstream in the hip can cause problems in the knee, knee pain and lack of motion can cause problems both up and downstream in the hip and foot/ankle. It’s better to get started correcting the problem in the knee versus allowing it to linger, creating problems above and below.
SO HOW DO WE DO IT?
Anyone starting an exercise program, young or old, knows what it feels like to start exercising. If you have OA of the knee it may be swollen, painful, and/or lack range of motion. With OA, too much of the wrong thing may cause more harm than good and definitely might cause someone to give up on exercise and look for a quick fix.
An exercise program for someone with OA of the knee should include compound movements for several reasons:
- they mimic functional movements (e.g. squat and deadlift)
- they disperse forces over multiple joints versus isolating the affected joint
- compound, closed-chain (foot grounded) exercises are superior to isolated, open-chain (foot not on the ground) exercises
But, compound movements ARE NOT the norm (unfortunately) and the educational opportunities for fitness professionals to learn them are not as prevalent as you might think. There are even physical therapists out there still teaching open-chain exercises for the knee as a primary strengthener for “functional movement”. It’s a sad state in the fitness world when clients, members, or in our case, “athletes” aren’t being given the opportunity to learn and grow into full range of motion, and functional movements. This is so wrong!
It goes without saying that too much of anything is a recipe for failure (exercise, food, sunlight). Too many repetitions and too much weight will generally increase pain and inflammation for an arthritic knee. The biggest concern in beginning an exercise program for someone with OA of the knee is creating more pain and inflammation – more symptoms – that may cause frustration and/or cause delays in progressing through the exercise program.
However, an exercise program WITHOUT functional movements like squatting or deadlifting doesn’t work. It is absolutely necessary so that participants are gaining strength in movements that they can use in their daily lives. Mainstream “everything” – programs, recommendations, equipment – are promoting the opposite. How often have we heard:
- My doctor said don’t squat – yet I’m supposed to get out of my car, off my chair and toilet – what’s the difference?
- The internet says low weights and high reps – yet high reps after no reps are a great recipe for inflammation and pain.
- My therapist has me doing “chair exercises” (seated exercises) – yet most of my life is not performed seated.
Compound, functional exercises that disperse weight through the ankle, knee, hip, low back, and core offset forces directly placed on the knee, which is easily irritated. These kinds of exercises strengthen the muscles around the knee as well as those above and below, contributing to better overall ability and balance.
Progress should be slow to avoid inflammation which can take time to subside, and therefore lose time otherwise committed to progress.
So where do we go from here?
SOLUTION: FIND A TRAINER, A FUNCTIONAL FITNESS PROGRAM, OR A CROSSFIT GYM
If you’re reading this, you’re probably already familiar with us. But if you share this, you’re sharing knowledge that might bring someone from incapable to capable – from weak to strong – or from in pain to out of pain! Don’t settle – here’s what a good program will do for you:
Experience matters – always. There’s only so much you can learn from a book. Heck, when we first started our first gym, we remember having the Olympic movement called the Snatch programmed, and watching YouTube videos all night because we “knew” the snatch, but how to coach it was something entirely different. Here, trainers “know” the squat (or sit to stand), but do they know how to coach someone with severe or even moderate, symptomatic OA of the knee without increasing their symptoms? Or do they know how to tell the difference between increased symptoms or what is going to happen when we start moving a formerly sedentary joint? Even easier, what about a “fussy” knee? We know the person has OA, but they’re not symptomatic all the time. Do you have them jump? Do you have them squat? The answers lie above in “where is the arthritis and where is the pain”.
Luckily, our program is seasoned, our trainers are educated and the founder is a physical therapist. However, this DOES NOT MEAN that without these credentials you can’t find a good gym or trainer to help you. It’s your job to interview them and ask a lot of questions. How many participants have they trained with OA of the knee? How many participants are your age? What is their education? Have they worked with seniors? What would their plan be for you?
So what will the program look like?
It will include a lot of strength training with dumbbells, kettlebells, and barbells. No – no machines. How often, unless you’re driving, are you “in a machine” doing laundry, gardening, or making dinner? Never, right? There are ways to teach you how to move correctly without a machine balancing part of the movement for you. A good trainer can break down and modify any and every movement to help you achieve the full functional movement over time. And you also get a “twofer” here. Functional movements often require good mobility. The squat opens the hips. The press requires full shoulder extension – even with a light stick overhead. And the deadlift (picking something up off the floor) requires the back of the leg (hamstrings) to be pliable. Functional movements beget mobility.
For example, the squat, or rather the “sit down and stand back up” if you need to communicate to your health care professionals…because they don’t like the work squat. We’re working on getting up and sitting down. The average chair is approximately 17″ high. That’s a good place to start if you’re comfortable. Your trainer will ensure you are positioned right in the seated position – feet a little forward (not back under the chair) and the weight in the midfoot and heels of your feet, not forward on your toes. Your trainer will cue you to push down into the ground with your heels, feel your butt squeeze and begin the “rise”. You may not make it, but this is step one. On day one, you may never fully rise from the 17″ (or higher) surface. You may just practice that (among other things). Your trainer is facilitating your butt, your core, and your legs somewhat to wake up and work first. That’s step one. Once that’s practiced, and easy, your trainer will progress you. The next day, you should feel “some” soreness in your butt, and your legs, but likely NOT your knees. You are patient and your trainer is patient and this is how progress is made.
A good trainer will tell YOU what your reps, loads, and position will be – you’ll comply. Eventually, you will play a role in choices, but initially, you trust your trainer and let them lead.
Other parts of your program may include pressing overhead, picking up off the floor (deadlifting), and core exercises. All of these are compound movements. Isolated accessory movements are legitimate accompaniments to compound movements, and they may be a part of your program.
Your program may also include things to get your heart rate up and make you breathe more heavily. Call it “cardio” if you wish, but it may last from 5 minutes to maybe 30 minutes. It’s not easy – not as easy as building strength at our age, but it’s necessary. Your heart is a muscle and it needs to be trained too. Plus, above we mentioned that one of the new and coming theories on what causes arthritis is more metabolic in type versus wear and tear. With that, a poor diet, with little movement, no strength training, and no cardiovascular work will contribute to arthritis pain and symptoms. So yes, a cardiorespiratory piece in your workout is necessary.
Finally, your program will include movements like calisthenics. Pushups are life-saving. If you can push yourself up off the floor from face down, and have the mobility to get into a half kneel and rise, you can recover from any fall, provided nothing is broken. And the same way a trainer professionally progresses these movements is the same way they progress those above. They break them down and modify the range of motion or the load – including your body weight. It’s truly amazing to see a 90-year-old woman do “Rx” or “boy” pushups – chest touching the deck without gut or legs, and pushing up to full extension. It happens. All the time!

SUMMARY
If you’re reading this, you’ve probably survived COVID and an economic monsoon of debacles and uncertainty. If we told you that you can make a difference in the quality of your life by heeding the advice we put forth here, why wouldn’t you make a move? You have to. We get one life, and it should be honored and lived well. Snap to it!

